The difference: endometrial cancer and uterine sarcoma
The difference: endometrial cancer and uterine sarcoma
Female cancers don’t get the kind of public attention that other cancers do. September is Women’s Cancer month, but you’re not likely to see many purple bands, fundraisers, or walks to raise awareness of the cause. Compared to breast cancer and its pink peak during Awareness Month in October, gynecological cancers — those of the cervix, ovaries, uterus (endometrium), vagina and vulva — are less well known.
Various symptoms and treatments.
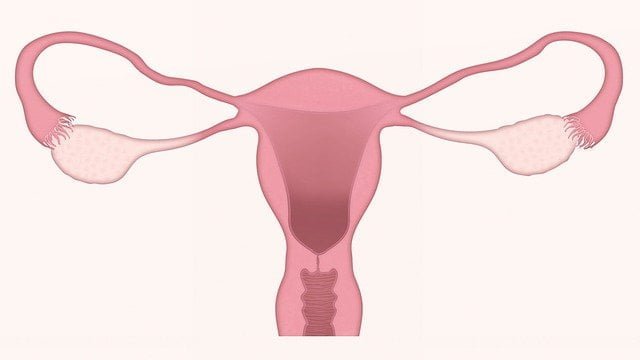
However, more than 100,000 women will be diagnosed with gynecological cancer in 2017, according to the American Cancer Society. Endometrial cancer is the most common cancer of the female reproductive system, but many women are unaware of the risk factors or symptoms of the disease. Here’s a tantalizing fact, for example: Because the endometrium is part of the uterus, it’s sometimes called endometrial cancer and more often uterine cancer. Endometrial cancer and uterine cancer are the same disease. But uterine sarcoma is a completely different entity with very different symptoms and treatments than uterine cancer.
When cancer forms in the lining of the uterus, it is called endometrial cancer. “This cancer is what’s known as adenocarcinoma, because it forms in the glands that secrete mucus,” says Dr. Justin Chura, MD, chief of surgery and director of gynecological oncology at our Hospital in Philadelphia. “Most uterine cancers are endometrial cancers.”
Meanwhile, uterine sarcoma forms in the uterine muscle. “Cancers that form in muscle, connective tissue, or bone are considered sarcomas,” Dr. Chura says. “Sarcomas are rare, so it’s important to get a second opinion from an expert.”
The risk factors for endometrial cancer and uterine sarcoma also differ. The main risk factors for developing uterine sarcoma include:
- Pelvic radiotherapy: Cancers that develop from this type of radiation exposure usually occur five to 25 years after treatment.
- Ethnicity: Uterine sarcomas are more common in African-American women than in Asian or white women.
- History of retinoblastoma : Women with this type of eye cancer have a higher risk of developing uterine sarcoma.”
Common risk factors
Common risk factors for endometrial cancer include:
- Age: Most women diagnosed with endometrial cancer are over 50 years old and have gone through menopause.
- Obesity: Because fatty tissue tends to produce higher levels of estrogen, being overweight increases the risk of endometrial cancer.
- Too many menstrual cycles – Menstruation exposes the lining of the uterus to estrogen, which builds up over time, so the longer the exposure, the greater the risk of the hormone stimulating abnormal cell growth. Women who started their periods before age 12 and those who went through menopause after age 50 are more likely to develop this disease. Also, late menopause may not carry an increased risk in women whose periods began later in their teens.
- No previous pregnancies: Women who have never been pregnant are more likely to develop endometrial cancer than women who have been pregnant at least once.
- Heredity: Lynch syndrome, also known as hereditary non-polyposis colorectal cancer, increases the risk of endometrial cancer. Women who inherit mutations in the BRCA genes or the PTEN gene may also be at increased risk.
- Estrogen replacement therapy: After menopause, replacing estrogen without increasing progesterone levels can increase a woman’s risk of developing endometrial cancer.
- Tamoxifen: Women who are being treated with this medicine for breast cancer have an increased risk of developing endometrial cancer.
The common symptoms of endometrial cancer and uterine sarcoma are similar.
| Common endometrial cancer symptoms include: | Common uterine sarcoma symptoms include: |
|---|---|
| Bleeding unrelated to menstruation | Unusual vaginal bleeding or spotting |
| Postmenopausal bleeding | Postmenopausal bleeding |
| Unusual vaginal discharge with no visible blood | Unusual vaginal discharge with no visible blood |
| Difficult or painful urination | frequent urination |
| Pain during intercourse | Abdominal pain |
| Pain and/or a mass in the pelvic area. | A lump (lump or growth) in the vagina. |
| Involuntary weight loss | Feel full all the time |
While these and other symptoms do not necessarily indicate uterine cancers, you should see your doctor for a checkup if you have them, as many types of uterine cancer are highly treatable if diagnosed early. Treatment options for endometrial cancer and uterine sarcoma are also similar. “Usually the initial treatment for both endometrial cancer and uterine sarcoma is surgery,” Dr. Chura says. “After surgery, the next step in treatment depends on the stage of the patient. Most patients with uterine cancer are stage I and require no treatment other than surgery. Uterine sarcomas, due to their aggressive nature, are often treated with chemotherapy after surgery. The type of chemotherapy depends on the type of Uterine sarcoma. Some uterine sarcomas can also be treated with hormone therapy.”



